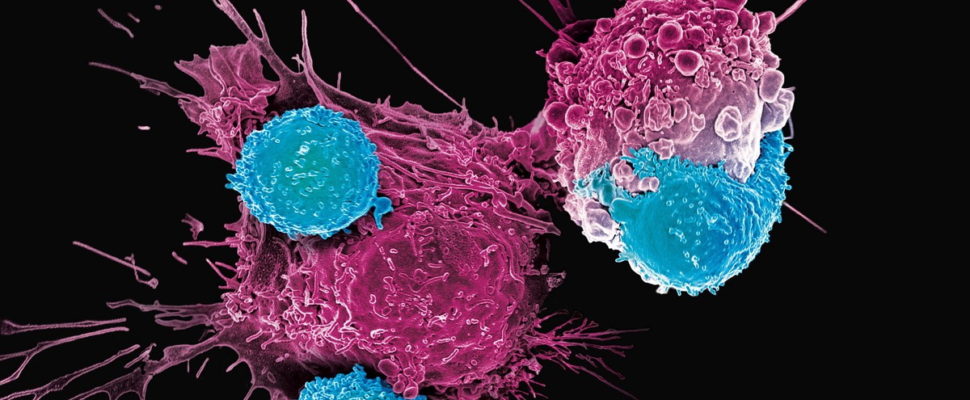
Most in oncology drug development are aware of the promise of immunotherapies – those in the clinic and the few now approved by the FDA, EMA and PMDA. T-cell transfer therapy is a very promising type of immunotherapy treatment that involves teaching healthy immune cells how to identify and destroy cancer cells.
T-cell transfer therapy can be referenced as adoptive cell therapy, adoptive immunotherapy, and immune cell therapy. There are two main types:
TIL therapy has shown some promising results in melanoma, but as of mid 2021, the treatments are still experimental. CAR T-cell therapies are further along, as there are currently three CAR T-cell therapies approved by the Food and Drug Administration for blood cancers:
There have been some notable breakthroughs in early 2021 with CAR T-cell research for solid tumors. Since numerous sponsors have been approaching Medelis to discuss these, we wanted to share a summary of the latest research in this article.
Early applications for CAR T-cell therapies focused on blood disorders. Solid tumor applications are different than hematological diseases for several reasons. One is the expression of a surface antigen that’s not expressed on normal tissues to avoid any organ toxicity. A second is that the tumor environment is highly suppressive. A third is called “T-cell exhaustion,” the concept that traditional CAR-T cells tire out when engaged in prolonged battles against a solid tumor.
However, in recent months, researchers are identifying antigens in solid tumors and conducting promising research, including
Here is a summary of each.
A novel chimeric switch receptor created at St. Jude Children’s Research Hospital significantly enhanced the effectiveness of chimeric antigen receptor (CAR) T cell immunotherapy in preclinical models of pediatric solid tumors.
The receptor, GM18, takes advantage of normal T cell activation and provides an additional signal to sustain the function of CAR-T cells. The CAR.GM18-T cells proved effective against solid tumors long after standard CAR-T cells have died.
In preclinical mouse models of osteosarcoma and Ewing sarcoma, the tumors shrank and disappeared in more than 90% of cases cell doses at which standard CAR-T cells were ineffective. Osteosarcoma and Ewing sarcoma are pediatric solid tumors. Outcomes have not improved for two decades for patients whose tumors have recurred or metastasized.
“The GM18 receptor also allowed CAR-T cells to function after repeated re-exposure to tumor cells, which had previously limited the effectiveness of the immunotherapy in treatment of solid tumors,” said corresponding author Stephen Gottschalk, M.D., chair of the St. Jude Department of Bone Marrow Transplantation and Cellular Therapy.
A potential CAR T-cell therapy by Innovative Cellular Therapeutics (ICT) showed early signs of safety and efficacy, significantly reducing tumor size in four patients with thyroid or colorectal cancer, new data show.
These findings were shared in two presentations on Friday, May 15, at the ongoing 23rd American Society of Gene & Cell Therapy Annual Meeting, held online this year because of COVID-19. The presentations are titled “CoupledCARTM Technology for Treating Thyroid Cancer” (page 554) and “Novel CoupledCARTMTechnology for Treating Colorectal Cancer” (page 555).
ICT generated CAR-T cells using a novel technology, called CoupledCAR, to overcome some of the limitations of current CAR T-cell therapies.
“CoupledCAR is ICT’s novel, in-house developed, proprietary CAR-T platform technology designed to overcome the challenges observed with conventional CAR-T therapies in treating solid tumors,” Larry (Lei) Xiao, PhD, founder and CEO of ICT, said in a press release.
Preclinical studies have shown that CoupledCAR significantly improved the cells’ proliferation and enhanced their ability to infiltrate tumors, inducing more potent anti-tumor responses.
Immunobiologists in China have designed a synthetic T cell receptor for anticancer therapy, engineering the protein not only with a capability to seek and destroy solid tumors, but endowing this cancer fighting weapon with potent endurance to get the job done.
The emerging technology additionally has been christened with a new name for solid tumor treatment. It’s called STAR T cell therapy, differing from its predecessor in the way it’s developed—with a synthetic receptor— and how it zeros in on cancer antigens by utilizing strong cell signaling activity. As with CAR T, STAR T cells are primed to hunt down tumor cells and kill the cancer.
The current form of treatment is composed of specially endowed cells that are engineered to destroy cancers of the blood. The emerging form of therapy promises the same powerful action—killing cancer cells, but this time from solid tumors while leaving healthy tissue unscathed.
Regardless of how the treatment is defined, CAR T cell therapy has been a groundbreaking form of treatment for B cell lymphomas and certain forms of leukemia. Children have been among the biggest beneficiaries because the therapy has been especially successful among youngsters compared with adults.
Yet, for either age group, solid tumors have eluded CAR T therapy’s ability to stop cancer in its tracks. Brain, breast, colon, lung and prostate malignancies have been impervious to the supercharged T cells. For these types of cancer, scientists say the emboldened T cells do not persist long enough to destroy tumor cells.
Immunotherapies that fight cancer have been a life-saving advancement for many patients, but the approach only works on a few types of malignancies, leaving few treatment options for most cancer patients with solid tumors. Now, in two related papers published April 28, 2021, in Science Translational Medicine, researchers at UCSF have demonstrated how to engineer smart immune cells that are effective against solid tumors, opening the door to treating a variety of cancers that have long been untouchable with immunotherapies.
In addition, both papers address the issue of so-called “T-cell exhaustion,” a long-standing challenge in which traditional CAR-T cells — the re-programmed intruder-hunting immune cells behind some of the most promising cancer immunotherapies — tire out when engaged in prolonged battles against the cancer. The new smart cells stay consistently strong through the entire fight, conserving their energy by switching to a standby mode when not directly engaged with the cancer.
“These findings address all critical challenges that have been in the way of developing immunotherapies for patients who suffer from these cancers,” said Okada, who also serves as director of the Brain Tumor Immunotherapy Center at UCSF. “This science is ready to move towards clinical trials.”
“We know that CAR T cells are safe for patients with solid tumors but so far they have not been able to cause significant tumor regression in the overwhelming majority of people treated,” said Jonathan S. Serody, MD, the Elizabeth Thomas professor of medicine, microbiology, and immunology and director of the immunotherapy program at UNC Lineberger Comprehensive Cancer Center. “Now we may have a new approach to make CAR T cells work in solid tumors, which we think could be a game-changer for therapies aimed at an appreciable number of cancers.”
In their published paper, which is titled, “STING agonist promotes CAR T cell trafficking and persistence in breast cancer,” corresponding author Serody, and colleagues, concluded: “To our knowledge, these data are the first to demonstrate the function of a STING agonist in altering the trafficking properties of adoptive T cellular products.”
The accumulation was particularly great when the mice were infused with CAR T cells that produce the immune signaling molecule IL-17A, compared with CAR T cells generated using standard techniques.
Serody and colleagues determined that the CAR T cells’ attack could be sustained for longer periods if the mice were also treated with therapeutic antibodies that deplete immunosuppressive cells from the tumor environment and prevent the immune checkpoint from deactivating the CAR T cells. The combination of all these approaches led to the complete eradication of breast tumors. “…sustained tumor regression was accomplished only with the addition of anti–PD-1 and anti–GR-1 mAb to Th/Tc17 CAR T cell therapy given with STING agonists,” the investigators wrote.
The team suggested that their findings point to a “viable strategy” for boosting CAR T activity in solid tumors. And while DMXAA, which worked well in the investigator’s mouse studies, has not provided benefit in human clinical trials as it does not activate human STING, the second STING agonist, cGAMP, does activate human STING and is known to boost the human immune system.
Colorectal cancer liver metastases (CRCLM) are a major source of morbidity and mortality. Historically, curative therapy has been limited to surgical resection, but only a small fraction of patients are eligible. Cellular immunotherapy has shown promise in hematologic cancers, but challenges to solid tumor therapy remain, including lymphocyte trafficking, elevated interstitial fluid pressures, and immunosuppression.
Regional intravascular infusion is a non-surgical, minimally invasive procedure commonly used in liver cancer to deliver therapeutics, which can be augmented by Pressure Enabled Drug Delivery (PEDD). We hypothesized that utilizing established regional delivery strategies to administer natural killer (NK) cells engineered to express a natural killer group 2, member D (NKG2D) activating chimeric receptor and membrane bound IL-15 (CAR NKG2D cells) could increase anti-tumor activity against liver cancer.
Since we’re in the early stages of studying CAR T-cell therapies in the clinic, many sites, CROs and clinical operations folks are still learning about the best approaches for keeping patients safe. As immunotherapy treatments become more prevalent, clinical teams will become more accustomed to handling the side effects.
Medelis has been at the forefront of this promising research, working with sponsors on promising phase I and phase II studies. In phase I, it’s critical to properly determine the dose. Cytokine release syndrome can cause life threatening side effects. Other serious side effects include:
Planning and continued communication are the keys to mitigating risk – to know what to watch for and communicate with the CRAs and cancer care team.
It’s also critical for the CRO or study management team to have the proper education and procedures in place to be able to recognize and treat these before they become life-threatening.
Learn more about Medelis’ immunotherapy experience in the below articles:
Managing the Side Effects in a CAR T-cell Therapy Study
Common Causes of Delays in Immuno-Oncology Studies
Therapies That Might Affect the Cancer-Immunity Cycle
Guidelines for the Evaluation of Immune Therapy Activity
Monitoring irAEs and SAEs in Oncology Immunotherapy Studies
Site Selection for Cancer Immunotherapy Studies
Contact us to discuss your study.